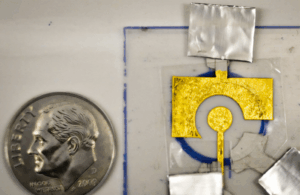
[Image courtesy of MIT]
MIT engineers have extended the shelf life of low-cost disposable DNA electrochemical sensors by sealing them with an inexpensive polyvinyl alcohol coating that keeps the devices stable for at least two months.
The coating on the sensors kept the devices stable in temperatures of up to 150°F. Researchers suggest that the technology could serve as a cheaper alternative for diagnosing diseases in low-resource regions, as the sensors cost only 50¢ to manufacture.
“Our focus is on diagnostics that many people have limited access to, and our goal is to create a point-of-use sensor. People wouldn’t even need to be in a clinic to use it. You could do it at home,” said senior author Ariel Furst, Paul M. Cook Career Development Assistant Professor of Chemical Engineering at MIT.
The study, led by graduate student Xingcheng Zhou, appeared June 30 in ACS Sensors. Co-authors are MIT undergraduate Jessica Slaughter, Smah Riki ’24 and graduate student Chao Chi Kuo. Funding came from the MIT Research Support Committee and a MathWorks Fellowship.
How the technology works
Each single-use sensor pairs a guide RNA with the CRISPR enzyme Cas12, and a handheld potentiostat reads the resulting change in current, similar to a glucose meter.
“If Cas12 is on, it’s like a lawnmower that cuts off all the DNA on your electrode, and that turns off your signal,” Furst said.
Earlier versions lost accuracy because the DNA layer degraded during storage. The research team addressed the issue by drying a thin polyvinyl alcohol film over the strands.
“Once it’s dried, it seems to make a very strong barrier against the main things that can harm DNA, such as reactive oxygen species that can either damage the DNA itself or break the thiol bond with the gold and strip your DNA off the electrode,” Furst said.
The polymer costs less than 1¢ per sensor. It covers DNA strands that are tethered to a gold-leaf electrode laminated onto plastic, holding the test’s total materials cost to about 50¢.
After storage, the protected sensors continued to detect PCA3, a prostate cancer marker found in urine. The same platform has previously identified HIV and HPV genetic material and can work with urine, saliva or nasal swabs.
What’s next?
A student team has entered MIT’s delta v accelerator to create a startup and commercialize the technology.
“Our goal is to continue to test with patient samples against different diseases in real world environments,” Furst said. “Our limitation before was that we had to make the sensors on site, but now that we can protect them, we can ship them. We don’t have to use refrigeration. That allows us to access a lot more rugged or non-ideal environments for testing.”
The team plans to develop disease-specific test panels, ship the devices without cold-chain constraints and validate performance in clinics and homes, especially in low-resource settings.

