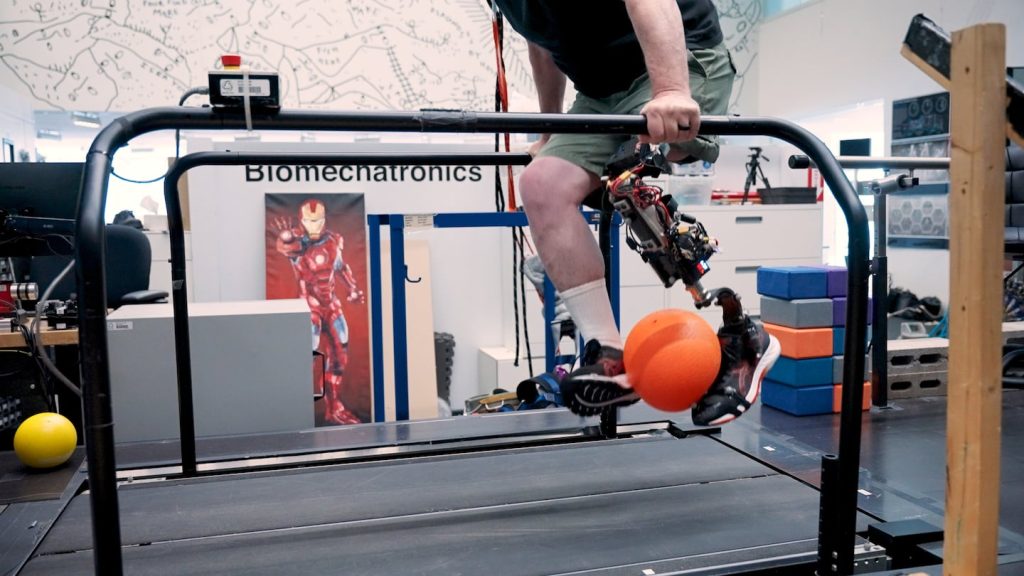
Now, because of a new bionic knee developed by MIT researchers, Gee, 63, has been able to kick a ball again and walk upstairs without having to stop on each step.
“I kept saying ‘I got my leg back!’,” Gee said of the prosthesis. “It wasn’t just a piece of hardware attached to my leg.”
Gee is one of 17 volunteers to participate in a clinical trial for the prosthesis, the results of which were published Thursday in the journal Science.
From January 2023 to early 2024, Gee traveled from his home in Litchfield, New Hampshire to MIT in Cambridge to spend four to eight hours testing out the prosthesis. The bionic knee is the first of its kind to integrate with a patient’s bones and nervous system, allowing users to control the prosthesis with their mind.
“In conventional prostheses, there’s an energy exchange, but there’s not much of an information exchange with the brain,” said Hugh Herr who co-leads the Yang Center for Bionics at MIT.
The tissue-integrated bionic knee is a big step forward for above-the-knee amputees who typically don’t have as many options for prostheses. Existing artificial limbs help with predictable movements like walking, but the bionic knee developed by Herr and Tony Shu, Herr’s former doctoral student, was intended to increase the wearer’s range of motion.
The prosthesis includes a permanent titanium rod inserted into the user’s thigh bone or femur. The rod is hollow and has 16 electrode wires that connect the removable part of the prosthesis to muscles in the thigh.
“Because the prosthesis is so intimately connected to the skeleton, if you just tap the toe in a really modest way, the person can feel it exquisitely,” said Herr, who is a double amputee himself.
The prosthesis also includes a small computer that translates muscle activity into movement. The math that bridges this gap is contained in only 500 lines of code, said Shu. The patient’s brain and the code work together to produce motion; Herr and Shu emphasized that they did not code distinct actions, like “dribble a ball.”
This approach provides the basic tools to generate movement while leaving creativity and control up to the patient, Shu said.
“We designed a very generic controller that codes general movements like flex the knee and extend the knee,” said Shu, lead author of the study, who completed his doctoral thesis in Herr’s lab in 2024.
The study involved putting three groups of volunteers with above-the-knee amputations through tests including walking up stairs, standing up without a handrail and avoiding a foam block obstacle when walking on a treadmill. One group, which served as a control, used the bionic knee without any other interventions. The two other groups underwent a surgical procedure developed by Herr and Dr. Matthew Carty of Brigham and Women’s Hospital that reconnects pairs of muscles that are typically severed during amputation. The muscles take turns stretching and contracting, conveying sensory information to the brain. The surgery, known as agonist-antagonist myoneural interface, or AMI, allows amputees to regain a push-and-pull dynamic in their leg muscles so that they have a vivid feeling of their phantom joint moving around.
Gee was in the only group to have the prosthesis fully integrated with their body with electrode wires going from the prosthesis into their thigh muscles. The other two groups used electrodes going from the skin surface of their amputated leg to the prosthesis to collect information about electrical activity of the muscles within their amputated limb.
The study found that patients who were using the bionic knee with electrodes implanted within their muscles could complete the tasks more accurately and with a greater feeling that the prosthesis was part of their body.
For example, Gee said that when he was starting to control the bionic knee, the sensation enabled him to know where his foot was in space, even when he was blindfolded as part of some of the experiments.
The results show that the success of the patients in Gee’s group is due not not only to the AMI surgery but also to the intramuscular electrodes and prosthetic bone anchoring working in tandem with the patients’ mind.
The study was funded by a federal DARPA grant awarded in 2017 and by the Yang Tan Collective at MIT, the MIT Media Lab Consortia and the National Science Foundation Graduate Research Fellowship Program. The prosthesis is not available commercially yet, but another graduate student is picking up where Shu left off and developing a responsive ankle to be included in the prosthesis.
Dr. Robert Gregg, a professor in the robotics department at the University of Michigan who also develops prostheses but was not involved in the current study, said that this study was the first time he’d seen AMI being implemented for above-the-knee amputees.
Gregg also said the study had integrated the prosthesis in an entirely novel way.
“What the MIT group has done is to directly tie into the nervous system to allow individuals to perform these volitional activities in a kind of similar way they would with their biological leg,” Gregg said.
Angela Mathew can be reached at angela.mathew@globe.com.